Chronic Renal Failure Condition is a Multifaceted Disease
We commend you for taking the time to read this report. It takes a very
special individual to delve into this field, as it’s often very challenging
to sort through all of the obstacles that accompany chronic renal failure (CRF)also known as
chronic kidney disease (CKD)
Unlike some illnesses, this condition is a multifaceted disease, which has many
complications that require a broad and integrative approach to treatment.
The journey is not easy, nor is the solution ever a straight line; but starting
with this e-book, we will do our best to help you navigate your way through
the difficulties.
As you read through the material, you may invariably come across information
that contradicts what you’ve been told. This is to be expected. Some of what
you are about to read will fly in the face of mainstream veterinary medicine.
Many conventional veterinarians will vehemently disagree with our conclusions.
 You must understand that some these individuals rely exclusively on their former
academic training and indoctrination, which might lack the lateral thinking
required to analyze and uncover developing research in emerging fields. On the
other hand, a true scientist is one who never stops learning; and who is willing
to thoroughly examine unfamiliar data before making a determination that is
based on logical deduction and conclusive evidence.
You must understand that some these individuals rely exclusively on their former
academic training and indoctrination, which might lack the lateral thinking
required to analyze and uncover developing research in emerging fields. On the
other hand, a true scientist is one who never stops learning; and who is willing
to thoroughly examine unfamiliar data before making a determination that is
based on logical deduction and conclusive evidence.
It is sad, but often true, that many an expert’s cup of knowledge is too
full for his or her own good. The best researcher is one who is always willing
to learn and evolve. That is the nature of progress. And progress is what real
science is all about. The good news is that there are a growing number of veterinarians
who recognize the value of integrative medicine. More and more professionals
are beginning to realize that the primitive band-aid approach is simply not
enough.
It should be noted that the data we present in this material, as well as
the information we offer throughout our website and online course, is based
on the cumulative and meticulous research of literally hundreds of some of the
world’s leading veterinary experts and medical scientists; whose clinical trials
have been published in peer-reviewed journals from all over the globe. In addition
to the aforementioned professionals whom we give credit, it may also interest
you to know that we are medical researchers ourselves; whose focus includes
kidney nutrition science.
The material you have before you is not comprehensive; nor is it meant to
be a shortcut or replacement for veterinary advice. Quite the contrary, as many
pioneering veterinarians have provided the foundation of what we discuss. It
is however, a report that is designed to inform you of the many dangers that
can arise from common decisions that people routinely make for their CRF pets.
Ultimately, it is our sincere hope that the information contained within these
pages—and the additional resources we have to offer—can help you find the answers
you’ve been searching for.

MISTAKE #1 Offering Tap Water
The Kidney is a Filter
 Most of us are aware that water has varying degrees
of purity and safety, depending on where it is derived; which may include
wells, city (tap) sources, and natural springs. In addition, this essential
resource can be found in forms that have been distilled or filtered by several
methods of purification.
Most of us are aware that water has varying degrees
of purity and safety, depending on where it is derived; which may include
wells, city (tap) sources, and natural springs. In addition, this essential
resource can be found in forms that have been distilled or filtered by several
methods of purification.
A few of us have decided to take things a step
further by investing in bottled water or sink and counter-top water filters; but for the most
part, very few individuals ever investigate exactly what is within the fluids
they consume, or the effectiveness of the measures they take to ensure safety.
Even if you are of the opinion that such concerns are unwarranted, when
it comes to the health of your CRF pet, nothing could be further from the truth.
Think of the kidneys as being similar to an aquarium charcoal filter.
For those of you who aren't familiar with these purification systems, like
renal tissue, this device is used to trap and remove impurities. If it fails
to do its job, replacement is required. Otherwise, it will be unable to
purify the water that is circulating within the fish tank. This results
in a build-up of ammonia, metabolites, nitrates, and other toxins. Like
the aquarium, when this process takes place within your pet's body, the
blood fails to become purified, and the entire system begins to deteriorate.
Unlike the typical aquarium filter, however, your pet's body is capable
of cleaning itself to varying degrees. Unfortunately, given the toxic nature
of the water most domesticated animals consume (as well as the entire multitude
of poisons found within pet food, medication, and the environment), it is
only a matter of time before the kidneys begin to degenerate.
This means that impure, contaminated water may be part of the reason that your pet has chronic
renal failure; and it certainly can contribute to further degeneration
of overall health. And assuming that your dog or cat does indeed have chronic
renal failure, it is crucial that from this day forward, your pet has only
the best water available.
Why Tap Water can not be assumed to be safe
Whatever you do, avoid the tap at all costs. The substances found in
most city water may actually contribute to CRF. You may wonder how this
could be, given the safeguards that regulatory agencies require. But the
sad truth is that these standards are not as safe as we are led to believe.
In the short-term, few studies have revealed enough evidence to state otherwise;
however, very little of the research can account for long-term health effects.
Unfortunately, when it comes to diseases that have developed over several
years, it is next to impossible to connect them to any specific cause, tap
water included. So, if that's the case, what evidence do scientists and
medical practitioners base their concerns? In order to understand the risks,
you must first understand the dangers associated with specific components
within the water. The following information covers only a fraction of what
can potentially be found in the drinking supply.
Heavy Metals that are known Toxins
Much of the piping that is used to run municipal drinking sources contains
heavy metals that are known toxins. In addition, the water itself is often
polluted with more of the aforementioned poisons, which have accumulated
from other origins. origins.
 Lead is a metal that is often found from the pipes and brass plumbing
in our homes. Even small amounts can accumulate in the tissues over time;
eventually leading to damage of the brain, kidneys, and bones. Chromium
is an industrial byproduct that can leach into the water supply; and has
been shown to cause respiratory issues. Cadmium, which can be found in zinc
fixtures and piping, can interfere with the proper absorption of key minerals
that animals require.
Lead is a metal that is often found from the pipes and brass plumbing
in our homes. Even small amounts can accumulate in the tissues over time;
eventually leading to damage of the brain, kidneys, and bones. Chromium
is an industrial byproduct that can leach into the water supply; and has
been shown to cause respiratory issues. Cadmium, which can be found in zinc
fixtures and piping, can interfere with the proper absorption of key minerals
that animals require.
Arsenic, which is used as rat poison, has actually
been discovered in trace amounts in some areas; and can lead to vomiting,
diarrhea, and cardiac conditions. Mercury is yet another metal that has
been found in municipal sources; and can accumulate in the body’s system
over time. Effects may include cognitive impairment, as well as kidney,
liver, and gastrointestinal complications.
Although aluminum is not listed on the U.S. Environmental Protection
Agency website as a toxin to monitor, it does lead to health complications,
and it has appeared in drinking sources. Patients with chronic kidney disease
that have not taken aluminum phosphate binders were still shown to have
elevated levels of this poison, since trace amounts can be found in the
water supply. Like mercury, aluminum is a neurotoxin, meaning that it can
kill brain cells.
Pesticides and Herbicides
The use of pesticides and herbicides has become so frequent, that it’s
almost impossible not to find these chemicals in tap water—and even some
bottled sources. They can lead to cardiac abnormalities, respiratory conditions,
organ degeneration; and have been linked to cancer over the long-term.
It may surprise you what is found in ordinary tap water
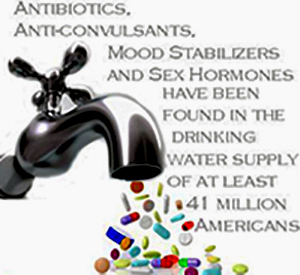 It may shock you to know what kind of
dissolved drugs are found in your city's drinking water.
Trace amounts of caffeine, growth hormones, birth control medication, antibiotics, anti-depressants,
and countless other prescription medicines have been found in tap water. Very
often, people flush their drugs down the toilet, where it passes through
obsolete filtration measures, to eventually end up recycled into our drinking
supply. A recent study funded by the Associated Press found that forty one
million Americans (not to mention countless animals) have been exposed to
various amounts of these chemicals. While it’s
not completely known what kinds of problems can occur from small amounts
of these drugs, there is no dispute that over time, these toxins accumulate
in the tissues of our bodies; and can certainly do the same for your pet.
It may shock you to know what kind of
dissolved drugs are found in your city's drinking water.
Trace amounts of caffeine, growth hormones, birth control medication, antibiotics, anti-depressants,
and countless other prescription medicines have been found in tap water. Very
often, people flush their drugs down the toilet, where it passes through
obsolete filtration measures, to eventually end up recycled into our drinking
supply. A recent study funded by the Associated Press found that forty one
million Americans (not to mention countless animals) have been exposed to
various amounts of these chemicals. While it’s
not completely known what kinds of problems can occur from small amounts
of these drugs, there is no dispute that over time, these toxins accumulate
in the tissues of our bodies; and can certainly do the same for your pet.
Chlorine leads to iodine and B vitamin deficiency
Chlorine is an inexpensive way for cities to cleanse and disinfect the
water supply. Unfortunately, high levels of this chemical can be found in
many municipal systems that are nearly comparable to what is found in the
average swimming pool. Chlorine leads to iodine and B vitamin deficiency;
and has also been found to be a major contributor to birth defects like
cleft palate and major brain defects. Excessive exposure can also lead to
cancer in pets and humans. Expectant mothers should stay clear of any water
that has high levels of this poison, to help eliminate the risk of these
conditions.
It is interesting to note that chlorine was
used in World War I and in Iraq as a chemical weapon. One of the
reasons it is so effective at killing germs is because of its ability to
destroy the outer cellular membrane. Now pause and think about this.
If chlorine wipes out live bacteria, what do you
think it's doing to the cells of your pet (or your own body for that matter)?
Fluoride is a Suspected Contributor of Renal Degeneration
All our lives, most of us have been repeatedly told how important
fluoride
is to our teeth and bones. Our dentists regularly advise us on the need
for adequate amounts of this “essential” nutrient. Our school teachers,
the media, and even those closest to us have all played a role in getting
us to recognize the need to make fluoride part of our daily life—because it's “healthy”.
But this mineral has a dark side that very few will ever come to know.
Although fluoride strengthens bones, it does so
by creating an abnormal skeletal structure that may ultimately cause calcification
of the joints (a disease known as fluorosis). It has also been considered
a suspected contributor of renal degeneration.
“Fluorosilicic acid [found in tap water]
may contain minute amounts of contaminants such as lead and arsenic.” -
American Dental Association (ADA)
The Facts Don't Lie
Although there are many claims that tap water is safe, the research shows
otherwise. According to the Environmental Working Group, more than
140 unregulated toxins were found in much of the drinking supply in just the United States alone.
Common dangers associated with tap water:
- Pesticides
- Herbicides
- Fungicides
- Chlorine
- Fluoride
- Lead
- Aluminum
- Mercury
- Cadmium
- Arsenic
- Prescription Drugs

MISTAKE #2 The Wrong Diet
The Hidden Dangers of Commercialized Pet Foods
In recent years, slick marketing campaigns have successfully enhanced
the image of today’s pet food. Carefully constructed commercials and labeling
strategies routinely employ the use of such terms as “scientifically formulated”,
“gold standard”, “premium protein”, “wholesome grains”, “superior health”,
and “fresh ingredients”. These words lull the masses into a false sense
of security.
The fact is, most commercialized dog and cat food brands contain indigestible
and substandard proteins, excessive amounts of grains, chemical preservatives,
elevated levels of acidity, and a variety of toxic byproducts.
Many of these substances can worsen the CRF condition;
and have likely played a significant role in the development of your pet's
current condition.
Our furry companion thrive on fresh, highly digestible, human-quality proteins
with nutrient rich water or “biological water,” which contains nutritional components found in meats and chicken broth.
This allows your cat to obtain moisture closer to the way a cat in the wild would get it.
Dr. Michael Dym DVM writes: "Over
the past 40 years and 17 generations of dogs and, cats we are seeing tremendous
increases in chronic ill health in our pets that was rare back in the early
1960's. Most of these illnesses revolve around breakdown in our
pets' immune systems, and include chronic skin/ear allergies, digestive
upset, thyroid/adrenal/pancreatic disorders, seizures, gum/ teeth problems,
degenerative arthritis, kidney/liver failure, and cancer across all ages
and breeds.
We are also seeing a record number of behavioral
and emotional disorders including alarming and unexplained fears/aggression.,
as well as difficulty focusing/training and paying attention. The analogy of these compared with escalating immune/behavioral diseases in children
is quite disturbing. The two biggest factors in our pets' population
health decline over these generations has been the severe overuse of
multiple vaccines and nutrient poor and toxin filled commercial pet foods.
We have also failed to address the underlying cause of disease by only suppressing
symptoms with antibiotics, cortisone and related drugs, so the disease progresses
and goes deeper. Homeopathy offers
a viable alternative in truly curing pets and making their bodies healthier."
Contaminated Protein Sources
 Many commercialized pet food brands claim to contain “premium” protein.
However, once you’ve traced these meats to their origins, you may think
twice before purchasing your pet’s favorite cat or dog food. Very often,
protein sources are given innocuous names to fool the uninformed. For example,
you will often see foods made with the following ingredients: “meat and
bone meal”, “beef and bone meal”, “fish meal”, “meat meal”, “meat by-products”,
“yellow grease”, “tallow”, “beef fat”, “chicken fat”, “animal fat”, and
“animal digest”.
Many commercialized pet food brands claim to contain “premium” protein.
However, once you’ve traced these meats to their origins, you may think
twice before purchasing your pet’s favorite cat or dog food. Very often,
protein sources are given innocuous names to fool the uninformed. For example,
you will often see foods made with the following ingredients: “meat and
bone meal”, “beef and bone meal”, “fish meal”, “meat meal”, “meat by-products”,
“yellow grease”, “tallow”, “beef fat”, “chicken fat”, “animal fat”, and
“animal digest”.
Your first reaction may be that all these food titles sound
good enough for your pet. However, nothing is further from the truth. According
to the U.S. Department of Agriculture, the ingredients used in manufacturing
do not require inspection. Certain laws allow the pet food industry to use what are referred to as “4D” sources; which
translates to any tissue that is dead, dying, disabled, or diseased.
These very same animal products are prohibited for sale to people, for they
are considered unfit for human consumption.
Risk of Pentobarbital in Dog Food
According to scientists at the University of Minnesota, the sodium pentobarbital
used to euthanize dogs and cats “survives rendering
without undergoing degradation.” In other words, the chemicals used to kill
terminally ill animals can be found in many pet foods today. In 2002, the
FDA published a report entitled, “Risk of Pentobarbital in Dog Food”. After
two years of investigation, they discovered the lethal drug in dog foods
purchased from grocery stores and retail outlets in Laurel, MD. Brand names
included Nutro, Ol’ Roy, Ken-L-Ration, Kibbles n’ Bits, and Purina Pro Plan,
among many others. No studies were conducted on cat food. It should be noted
that Laurel, MD is just one of many areas of the country that dog food suppliers
send their products to. If an investigation were to include cat food—and
if it were possible to involve every city in the nation—not to mention the
world—It wouldn’t take a genius to consider the magnitude of the problem
our pets face.
How it is that so many dangerous substances could be allowed to slip by undetected?
Other substances that find their way into rendering
plants include flea collars that contain antiparasitic chemicals, vaccinated
pet tissue, metal ID tags, surgical metal pins (used to mend broken bones),
and animal feces. Another problem includes plastic wrap, which cover many
of the unsold spoiled grocery meats that are thrown into the mix (as well
as the Styrofoam trays they are placed on). In addition, there are also
the antibiotics, growth hormones, and pesticides to consider.
You might wonder how it is that so many dangerous substances could be
allowed to slip by undetected. However, when you consider the enormity of
the situation, you will quickly realize how such circumstances routinely
occur. The animal rendering process is a multibillion dollar industry. Every
single day, millions of pounds of unused animal flesh are sent to these
facilities, which exist all around the U.S., Europe, and other parts of
the globe.
Although factory workers catch many of these poisonous materials,
it is simply not possible for them to find all of the indigestible matter
that is among the truckloads of carcasses that come their way. Plus, many
of the most toxic substances (that are within the animal) are simply not
visible to the naked eye. Combined with the rancid and indigestible leftover
parts taken from veterinary clinics, zoos, road kill, slaughter houses,
shelters, ranches, restaurants, and grocery stores, these contaminated meats
are then ground up, liquefied, and ultimately fed to the companions we all love.
“Feeding slaughterhouse wastes to animals increases their chance of getting cancer and other degenerative
diseases. Those wastes can include moldy, rancid or spoiled meats as well
as tissues severely riddled with cancer.” - Dr. P.F. McGargle (Veterinarian &
U.S. federal meat inspector)
In 2004, the Congressional
Research Center provided Congress a detailed report on the facts behind
the rendering industry, and their use of diseased, disabled, and euthanized
animals; many of which have become common ingredients in everything from
pet foods to soaps and crayons.
Another must-read article was provided by journalist Van Smith of the Baltimore City Paper in 1995:
It takes you directly into the heart of the rendering facility; and what
has been kept hidden from the consumer. Leftover meat scraps and
any unused animal parts began to be added to pet foods around the time of
World War II. Back then, very few people understood the nutritional requirements
of cats or dogs, and so the idea stuck for many years; and continues to
do so to this day. While recent years have brought many advances in animal
nutrition and veterinary research, we still have a long way to go before
most pet foods contain the kinds of protein that our companions need.
Carbohydrate Substitute
It’s important to see what potentially dangerous carbohydrates lurk
in pet foods. Many of these include byproducts of carbohydrate processing.
In other words, this is what’s left after the choice parts of the grains
have been removed; and are poor substitutes that may appear in your pet’s
food. Be on the lookout for brewers rice, cereal fines, feeding oatmeal,
and fermentation soluble. Also, overly processed carbs including maltodextrins
and soy flour are to be avoided at all costs. Other designations
to watch for include “potato products”. Although the title may seem benign,
quite often, this ingredient is composed of varying amounts of inedible
or rotten potatoes, french fries, chips, and skins; as well as fats or oils
that have been taken from frying operations.
Cheap Fiber - Examples include cellulose, corn bran, oat, and peanut hulls
Fiber is an important part of your pet’s diet. It helps clean out the bowels and supports
probiotics (friendly bacteria). Unfortunately, many sources of fiber are
not as beneficial as we’d like to believe; and are often used as cheap fillers
that do not aid in health. Examples include cellulose, corn bran, oat, and
peanut hulls. You’ll also want to steer clear of soybean and wheat mill
run, which are leftovers from grain processing. Much of the protein
that makes up pet food includes cereal grains such as corn, wheat, and soy.
The reason that they are added to most of these products is because they’re
used to increase the protein in the guaranteed analysis.
Over time, these grains cause stress to the internal
organs of the body; and can be especially harmful to the kidneys. In addition,
these same components are also known allergens, which often result in reactions
that prompt many pet parents to seek out drug treatments to alleviate the
symptoms. Usually, these food binders go by several nebulous or even
healthy-sounding designations, such as ground yellow corn, corn gluten meal,
whole grain corn, ground whole wheat, ground whole grain sorghum, and whole wheat flour.
Toxic Preservatives and Additives in Pet Foods
 Many preservatives and additives are included in pet foods to give them a longer shelf life. Research with lab
animals has shown a connection between many of these unnatural chemicals
and a variety of illnesses. While the evidence is still under further investigation,
a wise consumer should err on the side of caution, and seek nutrition that
does not contain risky substances. After all, we are talking about our beloved
companions; and they are not guinea pigs.
Many preservatives and additives are included in pet foods to give them a longer shelf life. Research with lab
animals has shown a connection between many of these unnatural chemicals
and a variety of illnesses. While the evidence is still under further investigation,
a wise consumer should err on the side of caution, and seek nutrition that
does not contain risky substances. After all, we are talking about our beloved
companions; and they are not guinea pigs.
Many of the chemicals used to preserve our pet foods have been linked to a variety of ailments. Take
ethoxyquin (EQ) for example. EQ is identified as a hazardous chemical by
the U.S. Occupational Safety and Health Administration (OSHA). There have
been documented cases of factory workers in the rubber industry who have
developed blindness, leukemia, skin cancer, fetal abnormalities, liver damage,
and kidney disease. Several studies with lab animals have shown that it causes DNA mutations, chromosomal aberrations, bladder
complications, and renal carcinogenesis; and significantly increases the
risk of stomach tumors and immune deficiency syndrome. But
this is merely one of many synthetic preservatives used in common pet foods.
Others include propylene glycol (PG), butylated hydroxyanisole (BHA), and
butylated hydroxytoluene (BHT); and they are no less poisonous. A whole
book could be written on all of the many toxic additives and preservatives
found in cat and dog food (not to mention our own); but such a task goes
beyond the scope of this report.
Many manufacturers will be quick to point out the fact that many studies include laboratory animals that
have been given excessive dosages; and that the levels that have been approved
for pet consumption have little to no evidence of danger. While short-term
research may not show a definitive correlation between these synthetic chemicals
and chronic disease, there simply is no way to know what the long-term ramifications
of eating these substances will be to an animal’s health. With a reasonable
dose of common sense, anyone can plainly see that the risks are simply not
worth it. Let’s not play Russian roulette with our pets.
“Since I have graduated from veterinary school in 1965, I’ve noticed a general deterioration in pet health. I believe
that the chemical additives in pet food play a major part in that decline.”
- Richard Pitcairn, DVM
Sweeteners are added to pet foods
Sweeteners are added to pet foods to make them more palatable. They are otherwise not
necessary, and can even be dangerous. Examples of these sweet poisons include
sugars from corn syrup, sucrose (table sugar), and molasses. The danger
lies in the overproduction of insulin, which over time causes cells to lose
their ability to pick up glucose from the blood. Adult-onset diabetes mellitus
then develops; which in turn can lead to a variety of health complications,
including kidney degeneration. Behavioral problems can also result, as we
often see in our children.
Related:
Sugar Substitutes - The Bitter Truth About NutraSweet (Aspartame) and Sucralose (Splenda)
Beautiful Toxins
While artificial colors may be attractive to humans, they have no place in pet
foods. Many artificial dyes are carcinogens, or cancer-causing agents. These
include FD&C Red #40 and sodium nitrite. Others, such as FD&C Yellow
#6, and Blue #1 and 2 impede the immune response, particularly in dogs that
are infected with the parvo virus. There are other food colorings that have
yet to undergo substantial laboratory testing to provide assurance of their safety.
Acidic Foods
Some health care practitioners are concerned about the over abundance of
acid-forming foods in diets. This could be particularly dangerous for
a pet with CRF that also suffers from metabolic acidosis. Avoiding products
that contain many of the disease-inducing ingredients listed in this module
can help restore normal pH balance.
Why Lowering Protein is Bad Advice
You may have been told that a reduced-protein diet is a necessary part
of an effective treatment plan for controlling CRF. This is because of the
statistical relationship between high protein and kidney degeneration. However,
this is an oversimplification of the facts. The truth of the matter is that
protein increases blood levels of phosphates and uric acid, which are the
real culprits behind the problem.
Another contributing factor is the specific type of protein that is used to meet dietary requirements.
There are several types of meats that contain substances known as purines,
which can cause complications in CRF pets, including elevated levels of
uric acid and the subsequent development of hyperparathyroidism (excess
parathyroid hormone). High-purine sources include animal organs, such as
the liver, kidneys, and brains; as well as some types of fish, such as sardines,
anchovies, mackerel, and herring.
 Together, the phosphates, uric acid, and uremia can all worsen kidney disease; which is the chief reason
so many vets recommend low-protein diets. However, the problem is that CRF
often leads to diminished appetites and muscle wasting. To offer reduced
amounts of protein will hasten the starving process.
Together, the phosphates, uric acid, and uremia can all worsen kidney disease; which is the chief reason
so many vets recommend low-protein diets. However, the problem is that CRF
often leads to diminished appetites and muscle wasting. To offer reduced
amounts of protein will hasten the starving process.
By default, low-protein diets may contain higher amounts of carbohydrates. If this is
the case, the extra carbs will produce spikes in insulin, which over time
can lead to diabetes—a disease that carries its own bag of problems, including
additional kidney damage. Remember, cats are obligate carnivores, and are
especially at risk because they cannot process carbohydrates as efficiently
as their canine counterparts. But even dogs require adequate levels of protein;
and this is especially true with those that are CRF patients.
Our Pets Are What They Eat
Remember, whatever is eaten, literally becomes a part of the body. The state of your companion's health is therefore
intrinsically connected to the quality of the foods you offer; which is
why it’s crucial to provide only the best nutrition available.

MISTAKE #3 Using Substandard Phosphate Binders
The Wrong Phosphate Binders: Good Intentions, Bad Approach
 More and more vets are beginning to realize that low protein diets and appetite stimulants are not the long-term
solution for dogs and cats that have lost the will to eat. Many professionals
now understand the need for effective phosphate binders to reduce the problems
associated with the protein these anorexic animals so often require. Unfortunately,
most of these treatments carry their own set of problems. Many of them contain
harmful substances like aluminum and other ingredients contraindicated for
pets diagnosed with CRF.
More and more vets are beginning to realize that low protein diets and appetite stimulants are not the long-term
solution for dogs and cats that have lost the will to eat. Many professionals
now understand the need for effective phosphate binders to reduce the problems
associated with the protein these anorexic animals so often require. Unfortunately,
most of these treatments carry their own set of problems. Many of them contain
harmful substances like aluminum and other ingredients contraindicated for
pets diagnosed with CRF.
Aluminum-Based Binders
There are a number of phosphate binders on the market based on aluminum.
Examples include aluminum hydroxide (Alternagel, Alu-Cap, Alu-Tab, Amphojel,
Basaljel, Dialume, Spectrum) and aluminum magnesium hydroxide (Aludrox,
Maalox, Milk of Magnesia, Mylanta). While they are effective in reducing toxins within the blood,
it is important to understand that there are serious
trade-offs. The metal has been shown to accumulate in the brain, leading
to bizarre behaviors, neuron destruction, memory problems, and even death.
Research has demonstrated that even a few doses can cause permanent damage.
Furthermore, aluminum builds up in the bone, causing further issues with anemia.
Calcium-Based Inhibitors
PhosLo is an example of a phosphate binder that contains calcium. Many pet owners
observe that it is unreliable and can have variable effects. Also, it may
add too much of this mineral to the blood, which may result in calcification
(hardening) of tissues. It is important to have your vet check calcium and
phosphorus levels frequently if your pet is on PhosLo. Additional side effects
may include allergic reactions and interactions with other medications.
Your veterinarian may also recommend other phosphate binders in this
category, such as ground-up eggshells or the like. Although these may be
natural treatments, they may still initiate elevations in blood calcium.
“Aluminum and calcium-containing phosphate binders have been increasingly abandoned—the former because of
their influence on bone (low turnover) and the brain (dementia), and the latter because
of the increased frequency of vascular calcification.”- Martin Haas, MD
Lanthanum-Based Inhibitors
New technology has incorporated the rare metal, lanthanum for phosphate control. Renalzin and
Fosrenol are two examples. Unfortunately, these drugs can trigger nausea,
vomiting, intestinal blockage, and abdominal pain. They have not been tested
extensively in cats and dogs; so there may be additional issues that researchers
have yet to uncover. Some scientists vigorously defend the safety of lanthanum;
but with the dangerous reputation it has for accumulating in the lungs and
bones, it may not be worth risking.
Polyamine-Based Phosphate Binders
This class of drug was developed as an alternative
to aluminum-based binders. Polyamines have a positive charge that attracts
negatively-charged phosphate molecules. Once the binder has accomplished
its task, the threat is dispelled from the digestive tract. Sevalamer
(Renagel) is a polyamine that has been shown to bind phosphates without
raising calcium levels. Still, it has a host of side effects; including
constipation, allergic reactions, nausea, vomiting, and breathing difficulties.
This drug should never be given to an animal with stomach or intestinal
problems, since it can result in perforation of the gastrointestinal tract.
It may also react with other medications; and has been shown to reduce vitamins
D, E, K, and folic acid in the body, when given long-term.

MISTAKE #4 Resorting to Appetite Stimulants
Disabling the Oil Light Doesn’t Fix the Leak
 If your dog or cat has lost his or her appetite, and has
begun to lose weight, steps must be taken to remedy the situation as quickly
as possible. Unfortunately, the treatment of surface symptoms is often the
only approach. In the case of anorexia, appetite stimulants are usually
the remedy of choice. You must understand that these drugs fail to
address the cause of the problem. There is a reason CRF pets lose the desire
for food. Dehydration is often the culprit; as is the toxic accumulation
of metabolic wastes (such as ammonia and phosphates). Forcing the animal
to eat without eliminating the symptom’s trigger is a temporary fix at best;
and is a highly toxic threat at worst. Ignoring the origin of disease only perpetuates it.
If your dog or cat has lost his or her appetite, and has
begun to lose weight, steps must be taken to remedy the situation as quickly
as possible. Unfortunately, the treatment of surface symptoms is often the
only approach. In the case of anorexia, appetite stimulants are usually
the remedy of choice. You must understand that these drugs fail to
address the cause of the problem. There is a reason CRF pets lose the desire
for food. Dehydration is often the culprit; as is the toxic accumulation
of metabolic wastes (such as ammonia and phosphates). Forcing the animal
to eat without eliminating the symptom’s trigger is a temporary fix at best;
and is a highly toxic threat at worst. Ignoring the origin of disease only perpetuates it.
Let’s use an automotive example to illustrate our point. If a vehicle’s oil light is flashing, an
intelligent person addresses the cause and refills the fluid. Masking the
problem by disabling the warning signal doesn't solve anything. Quite often
the reverse is true. While some symptoms should be treated directly (particularly
if they are life-threatening or causing extreme stress); we must always
attempt to address the cause. Only then can we make lasting change that
is best for the health of our pets.
Acid-Suppression Drugs
Famotidine (Pepcid AC), Cimetidine (Tagamet), Ranitidine (Zantac), Nizatidine
(Axid), and Omeprazole (Prilosec) are all drugs that have the ability to
reduce the secretion of acid; subsequently increasing appetite. Some of
these treatments may lead to dangerous urinary tract infections; and could
harm the brain and nerves, as well as the liver. These drugs can also make
kidney disease worse. Cyproheptadine (Periactin) is an example of
an antihistamine that makes animals hungry. Unfortunately, like the aforementioned
drugs, these come with adverse effects, including aggressive behavior in
cats. Dry mouth and sedation may also occur. Don’t use Periactin if your
pet has heart disease, glaucoma, intestinal blockage, or prostate enlargement.
Anti-Anxiety Drugs
Diazepam (Valium) and Oxazepam (Serax) increase appetite. They tend to work better in cats than dogs. Unfortunately,
these drugs not only have the potential of causing a lack of coordination—which
can be dangerous—they may also induce tremor and edema (retention of water).
Some companion animals may also experience liver failure and kidney damage.
Some specialized tranquilizers, such as Acepromazine (Atravet), Chlorpromazine
(Thorazine/Largactil), and Prochlorperazine (Compazine), have been used
to reduce vomiting. Adverse reactions may include seizures, dangerously
low blood pressure, and excessive lethargy. Don’t use tranquilizers with
any insecticides, such as flea or tick dips, collars, or powders.
Anticholinergic Drugs
These drugs include Aminopentamide (Centrine), Hyoscyamine/Phenobarbitol (Donnatal), Hyoscyamine (Levsin),
Clinidium/Chlordiazepoxide (Librax), and Methscopalamine (Pamine). Unfortunately,
anticholinergics can cause urine to be retained in the bladder. They can
lead to constipation, light sensitivity, confusion, cardiac arrhythmias,
and lethargy. These effects could be very dangerous in an animal that is
already sick, so they are contraindicated in pets with CRF.
Dopamine Antagonists
Another drug that may prevent vomiting includes Metoclopramide (Reglan). This works to block nausea signals
within the brain. It should not be given to pets with kidney or liver disease,
adrenal problems, or seizure disorders. This medicine can also cause abnormal
movements of the mouth and tongue due to a brain disorder known as tardive dyskinesia.
Serotonin Blockers
Dolasetron (Anzemet) and Odansetron (Zofran) prevent the chemical messenger molecule
serotonin from being released, which sometimes decreases vomiting. These
drugs are not always effective in blocking sensations of nausea. They may
also cause issues with the heart.
Steroids can all cause serious problems
There are several classes of steroids that have been used to increase
appetite. Not surprisingly, they can all cause serious problems—none of
which can a CRF pet afford. While anabolic steroids can be used to
stimulate appetite, they are not recommended, due to their potentially life-threatening
side effects; which may include liver and kidney failure. Stanozolol (Winstrol-V)
is an example of this type of medication. Progestins such as Megestrol
Acetate (Megace) are a type of progesterone (a hormone found in female animals).
Unfortunately, they may lead to a degeneration of the adrenal glands and
the development of diabetes. This drug should not be used in pets with uterine
problems or cancer of the mammary glands. It should also be avoided in CRF
patients. Glucocorticoids are another class of steroids that have
been shown to increase the desire to eat. A common example includes prednisone.
These drugs can lead to serious complications, including diabetes and heart
failure. They suppress the immune system; and can break down normal tissue
to increase blood sugar—which is dangerous if your pet has already lost
a significant amount of weight.
Dr. Jeffrey Levy - "
Corticosteroids (cortisone-type anti-inflammatory drugs) are the
most abused and dangerous class of drugs. Not only do they not cure
the underlying cause of the problem, they usually make the underlying
problem, that is, the real problem, worse"
Assisted Feeding: A Temporary Fix—Without the Toxic Effects
You may want to try assisted feeding. This one strategy is
often enough to hold starvation at bay, until the problem is controlled.
It is relatively easy to learn, has no adverse effects, and has literally
saved thousands of lives. However, it should be
noted that if a nauseated animal cannot hold food down, this method may
not be effective. For such instances, the cause, which is likely to be uremia
or dehydration (or other related issues), must first be managed.

MISTAKE #5 Treating UTIs with Antibiotics
The Questionable Use and Abuse of Antibiotics
 Quite often, CRF pets will develop urinary tract conditions that lead to infections. Sometimes, this may be due to
crystallized stones that have developed as a result of pH imbalances within
the diet. In addition, degenerated kidneys eventually fail to maintain proper
concentration levels of urine; which increases the likelihood of bacterial
invasion. These challenges can only complicate things for cats and dogs
diagnosed with chronic renal disease.
Quite often, CRF pets will develop urinary tract conditions that lead to infections. Sometimes, this may be due to
crystallized stones that have developed as a result of pH imbalances within
the diet. In addition, degenerated kidneys eventually fail to maintain proper
concentration levels of urine; which increases the likelihood of bacterial
invasion. These challenges can only complicate things for cats and dogs
diagnosed with chronic renal disease.
Antibiotics Kill the Good with the Bad
When a urinary tract infection (UTI) arises,
veterinarians will often prescribe antibiotics to quickly eliminate the
threat, under the assumption that such measures will prevent more severe
symptoms from developing. Unfortunately, there are a whole host of problems
associated with these drugs that most people are not aware of.
One legitimate concern is the fact that these medications not only kill disease-causing
pathogens, but they also destroy the beneficial flora that are vital to
the intestinal health of your pet. When the friendly bacteria are reduced
in strength and numbers, yeast infections are able to take over the body,
further taxing the animal’s delicate immune system.
What Does Not Destroy Bugs Makes Them Stronger
As the use of antibiotics increases,
the destructive bacteria can develop a resistance; making it more difficult
to treat infections. Scientists have discovered that these microbes have
the ability to avoid being destroyed by these drugs through the use of a
layer of protection known as biofilm. While these organisms are protected
within the digestive tract, their DNA mutates to combat the antibiotic.
When these “superbugs” have become resistant to the drug, stronger, more
toxic treatments will often be required to deal with the recurring infection;
which can become a losing proposition for the feline or canine patient.
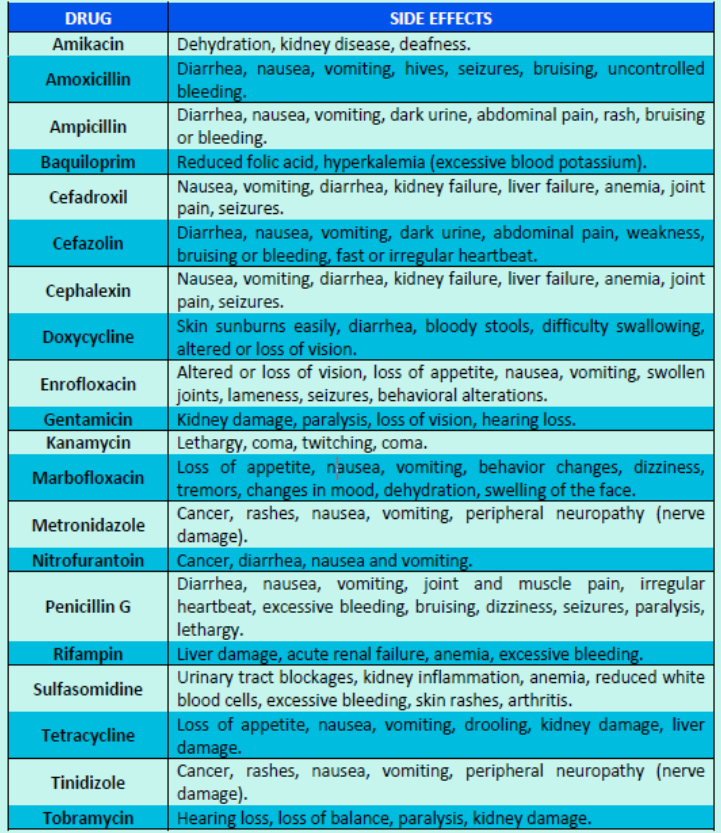
The Toxic Effects of Antibiotics
Emerging evidence of serious side reactions has been associated with the use of antibiotics.
One of these effects is the degeneration of the body’s nerves, which can
result in a painful condition known as peripheral neuropathy. These drugs
have also been shown to lead to anemia, platelet loss, and compromised immune
function. They can also destroy the kidneys and liver; and in documented
cases have even led to brain damage.

MISTAKE #6 Synthetic EPO Therapy
The EPO Gamble
 Erythropoiesis-stimulating agents (ESA) are genetically engineered,
protein-based human hormones given to pets
to help produce red blood cells from the bone marrow. Some examples on the market
include Aranesp, Epogen, Eprex, NeoRecormon, Procrit, rfEPO, and rhEPO. This
protein is given to animals via injection up to three times a week, depending
on the veterinarian’s directions. The remedy begins to work within a day; but
most studies have shown that pets return to normal blood cell levels after four
weeks of consistent therapy.
Erythropoiesis-stimulating agents (ESA) are genetically engineered,
protein-based human hormones given to pets
to help produce red blood cells from the bone marrow. Some examples on the market
include Aranesp, Epogen, Eprex, NeoRecormon, Procrit, rfEPO, and rhEPO. This
protein is given to animals via injection up to three times a week, depending
on the veterinarian’s directions. The remedy begins to work within a day; but
most studies have shown that pets return to normal blood cell levels after four
weeks of consistent therapy.
Fatal Reaction
Although exogenous human erythropoietin has been used for cats and dogs, it isn’t recommended,
since an animal’s immune system may interpret the human proteins as foreign;
and can react by destroying them. What’s worse is that in most cases, the antibodies will not only target
the human-based hormone, they will often attack their own native blood as well;
inevitably leading to irreversible anemia. In one study of artificial human
EPO, two out of three dogs treated for more than 90 days, and five out of seven
cats given treatment for twice that time, developed a type of rebound, incurable
anemia. If this occurs, from that point forward, the only known course
of action that could save the animal would be a blood transfusion—which has
its own set of risks—and if successful, would only offer temporary results.
Veterinary science is attempting to create feline and canine versions of synthetic erythropoietin;
however, even if the proper animal form has been successfully developed, it
may not be the answer pet parents are looking for. In one trial, cats that were
given experimental feline EPO showed that over a quarter of them developed deadly
antibodies. In many cases, the use of synthetic erythropoietin will offer
only temporary results; and is often the beginning of the end. Since this treatment
has as high as a one in four chance of triggering a fatal form of anemia, we
would recommend its use only as a last resort—if at all.
Related: Animal recovery from Autoimmune Hemolytic Anemia

MISTAKE #7; Giving Up Too Soon
Facing the Crossroad
 By the time pets show signs of chronic renal failure, they may have lost as much as 2/3 of their original
kidney function. Over time, this degenerative disease contributes to a poisonous
build-up of metabolites which lead to additional complications (such as uremia
and secondary hyperphosphatemia).
By the time pets show signs of chronic renal failure, they may have lost as much as 2/3 of their original
kidney function. Over time, this degenerative disease contributes to a poisonous
build-up of metabolites which lead to additional complications (such as uremia
and secondary hyperphosphatemia).
These toxic by-products lead to compromised
immunity, nausea, reduced appetite, and chronic dehydration; all of which further
impair kidney function, invariably leading to greater damage. Once this chain
of destruction becomes severe, your dog or cat may have what is often referred
to as a “crisis”. At this point, the situation becomes a true medical emergency;
and immediate response is required in order to save the life of your pet.
Fatal Advice
Unfortunately, there are some veterinary
doctors who have seen so much disease and death, that hopeful expectations are
often replaced by cynical resignation. If you suspect that you are dealing with
this type of person, you may need to go elsewhere. Quite often, these individuals
may advise you to euthanize your pet, in the belief that doing so would save
the both of you unnecessary hardship that the vet is all too familiar with.
While such a recommendation is usually motivated by good intentions, the veterinarian’s
experience may be based on treatment solutions that are outdated and ineffective.
He or she may not be familiar with innovative strategies that have kept
many CRF pets alive and healthy for months, and sometimes years after their
initial diagnosis and predicted demise. Keep this in mind if euthanasia is the
first thing the veterinary specialist recommends. Pessimism is not realism.
If you're told that euthanasia is your only option, get another opinion.
IV Fluids May Reverse a Crisis
If your cat or dog is in an emergency situation, and your veterinarian has recommended intravenous
(IV) fluid therapy, it would be wise to consider doing so. After all, there
are many documented cases in which an animal has been in crisis, and the administration
of this treatment has literally saved his or her life. Intravenous fluids
are specially balanced with the correct amount of electrolytes, composed of
essential minerals, such as sodium, potassium, and chloride, which keep the
body running smoothly. This therapy is beneficial because the procedure dispenses
vital fluids directly into the veins; which facilitates rapid distribution to
the entire body. As the animal becomes rehydrated, the kidneys are able to effectively
remove toxins, which will undoubtedly make your pet feel a whole lot better.
Likewise, IV fluids may also be used to dispense life-saving medications
that can be delivered quickly and efficiently. While we don't typically recommend
the regular use of conventional drugs to treat chronic disease, there are definitely
cases where certain medicines can intervene in near-death emergencies.
Even if all hope seems lost, if IV fluid therapy is an option, you may want
to take it before you consider euthanasia.
If the laboratory values don’t significantly improve, you can at least have the assurance that you tried everything you could
to reverse the crisis. However, in many cases, lab numbers do indeed change,
and often for the better. It is a temporary reprieve; but it can give you the
time you need to optimize your treatment plan and improve your pet’s health,
with the hope that doing so will prevent a recurrence.
It is important to note, though, that IV fluid therapy will not always
be the wisest route. If your vet notices that your pet’s blood test results
show severe anemia, this treatment would be contraindicated. Excess fluid levels
may cause the blood to become so diluted that oxygen will be unable to reach
the body’s tissues. This is why it’s important to keep a regular eye on lab values.
Taking preventative measures and observing your pet's
day-to-day behavior may help circumvent the need for IV fluids in the first
place. Finally, it must be noted that this treatment is usually reserved only for life-threatening situations. For if this
therapy is given too frequently, it can become taxing to the kidneys; potentially
leading to additional renal damage.
Don’t Give Up
Fluid therapy is only one of many strategies that you may need to mitigate
the effects of CRF. In fact, effective long-term treatment
for this disease requires a multifaceted approach that demands the right knowledge
and resources for the job . Not only must you find a good veterinarian,
but you must also conduct your own research—beyond what is in this report. The
task is not easy—and few are willing to embark on this journey. You might
wonder, is the struggle worth it? It is our fervent belief that it is.
We don't euthanize people who are diagnosed with kidney
disease. We do what we can to preserve their lives and make their time
on this Earth worthwhile. Should we do any less for the companions we love?
Euthanasia has its place. But the question is, at what point is it necessary?
Make no mistake, with CRF, there will be times of discomfort—both for you and
your pet. But for every moment suffered, there are many more that can be invested
in warmth, affection, and love; all of which will be treasured for life.

Resources and References
Adams LG, Polzin DJ, Osbourne CA, O’Brien TD, Hostetter TH. Influence of dietary protein/ calorie
intake on renal morphology and function in cats with 5/6 nephrectomy. Lab Invest.
1994; 70: 347-57.
Albaaj F, Hutchison AJ. Phosphate control in renal
disease. Europ Renal Dis. 2007.
Amerling R. Treatment of phosphorus
and calcium disorders in chronic kidney disease. US Kidn Urol Dis. 2005.
Bassil KL, Vakil C, Sanborn M, Cole DC, Kaur JS, et al. Cancer health
effects of pesticides: Systematic review. Can Fam Physician. 2007; 53(10): 1704-11.
Becker GS. Animal rendering: Economics and policy. CRS Rep Congr. March
17, 2004.
http://digital.library.unt.edu/ark:/67531/metacrs9085/m1/1/high_res_d/RS21771_2004Mar17.pdf
.
Brown SA, Crowell WA, Brown CA, Barsanti JA, Finco DR. Pathophysiology
and management of progressive renal disease. Vet J. 1997; 154: 93-109.
Chan G, Steddon S, Goldsmith D. Redefining efficacy in contemporary phosphate
control. European Renal Dis. 2007.
Chertow GM, Raggi P, McCarthy
JT, et al. The effects of sevelamer and calcium acetate on proxies of atherosclerotic
and arteriosclerotic vascular disease in hemodialysis patients. Am J Nephrol.
2003; 23(5): 307-14.
Cohen JS. Peripheral neuropathy associated with
fluoroquinones. Ann Pharmacother. 2001; 35(12): 1540-7.
Cohen S, Kimmel
PL. Nutritional status, psychological issues and survival in hemodialysis patients.
Suzuki H, Kimmel PL (eds). Nutrition and Kidney Disease: A New Era. Basel: Karger,
2007.
Committee on Minerals and Toxic Substances in Diets and Water for
Animals, National Research Council. Mineral Tolerance of Animals. 2nd revised
ed. Washington, DC: National Academies Press; 2005.
Costerton JW, Stewart
PS, Greenberg EP. Bacterial biofilms: A common cause of persistent infections.
Sci. 1999; 284: 1318-22.
Cowgill LD, James KM, Levy JK, Browne JK, Miller
A, et al. Use of recombinant human erythropoietin for management of anemia in
dogs and cats with renal failure. J Am Vet Med Assoc. 1998; 212(4): 521-8.
De Broe ME. Debunking the Myths About Lanthanum Toxicity: An Expert Interview
With Marc E. De Broe, MD, PhD.
.
Dunn TJ. Pet medications…antibiotic use and misuse.
Eife R, Weiss M, Barros
V, Sigmund B, Goriup U, et al. Chronic poisoning by copper in tap water: II.
Copper intoxications with predominately systemic symptoms. Eur J Med Res. 1999;
4(6): 224-8.
Environmental
Working Group Web site. National Tap Water Quality Database.
Finch
CA. Erythropoiesis, erythropoietin, and iron. Blood. 1982; 60(6): 1241-6.
Fluoride Action Network Web site. http://fluoridealert.org/.
Gibbs BF, Mulligan CN. Styrene toxicity: An ecotoxicological assessment.
Ecotoxicol Environ Safety. 1997; 38(3): 181-94.
Grauer GF, Bartges JW,
Sunvold GD. Management of Chronic Renal Failure. Presented at the North American
Veterinary Conference. Dayton, OH: The IAMS Company; 2000.
Jo WK, Weisel
CP, Lioy PJ. Chloroform exposure and the health risk associated with multiple
uses of chlorinated tap water. Risk Analy. 2006; 10(4): 581-5.
Ketteler
M. Phosphorus control in chronic kidney disease. European Renal Dis. 2007.
Kutlubay R, Oguz EO, Guven C, Can B, Sinik Z, et al. Histological and
ultrastructural evidence for protective effects on aluminium-induced kidney
damage by intraperitoneal administration of -tocopherol. Int J Toxicol. 2007;
26(2): 95-101.
Lite J. Warning: If antibiotics don’t work, don’t take
them.
http://www.sciam.com/blog/60-second-science/post.cfm?id=warning-if-antibiotics-wont-work-do-2008-10-02
.
Loghman-Adham M. Adaptation to changes in dietary phosphorus intake
in health and in renal failure. J Lab Clin Med. 1997; 129(2): 176-88.
Maddison JE, Page SW, Church DB. Small Animal Clinical Pharmacology. Maryland
Heights, MO: Elsevier Health Sciences; 2001.
Merck Veterinary Manual
Web site. Toxicology: Introduction..
Nicholas RB, Freide AI. Perspectives
on bacterial resistance and veterinary-use antibiotics.
North Carolina State
University Water Quality Group Web site. http://www.water.ncsu.edu/watershedss/info/hmetals.html.
Payment P. Epidemiology of endemic gastrointestinal and respiratory diseases:
Incidence, fraction attributable to tap water and costs to society. Water Sci &
Tech. 1997; 35(11-12): 7-10.
Petplace.com Web site. Warning: Is tap water
safe for your dog?
http://www.petplace.com/article/dogs/news-videos-fun/news/warning-is-tap-water-safe-for-your-dog
.
Pitcairn RH, Pitcairn SH. Dr. Pitcairn’s Complete Guide to Natural
Health for Dogs & Cats. 3rd ed. Emmaus, PA: Rodale Press; 2005.
Prescott
JF, Baggott JD, Walker RD. Antimicrobial Therapy in Veterinary Medicine. Ames,
IA: Iowa State University Press; 2000.
Prie D. Control of phosphate.
European Real Dis. 2007.
Pruchnicki MC, Coyle JD, Hoshaw-Woodard S,
Bay WH. Effect of phosphate binders on supplemental iron absorption in healthy
subjects. J Clin Pharmacol. 2002; 42(10):1171-6.
Randolph JF, Scarlett
JM, Stokol T, Saunders KM, McLeod JN. Expression, bioactivity, and clinical
assessment of recombinant feline erythropoietin. Am J Vet Res. 2004; 65(10):
1355-66.
Ranganathan N, Friedman EA, Joseph A, Delano B, Goldfarb DS,
et al. Probiotic dietary
supplementation in chronic kidney disease (CKD III
and IV) – Preliminary observations and combined data analysis of a 6-month pilot
scale, randomized, double blind and crossover study design in Argentina, Canada,
Nigeria, and USA.
Reddy DR. Neurology of endemic skeletal fluorosis. Neurol India.
2009; 57: 7-12.
Ryder MA. Biofilm: Biofilm recalcitrance to antimicrobials.
Smith MK, George EL, Zenick H, Manson JM, Strober JA. Developmental
toxicity of halogenated acetonitriles: Drinking water by-products of chlorine
disinfection. Toxicol. 1987; 46(1): 83-93.
Smith V. What’s cookin’? Ever
wonder what happens to dead animals? A look at Baltimore’s only remaining rendering
plant explains. City Paper. September 29, 1995.
http://www2.citypaper.com/about/vansmith.asp
.
Suzuki KT, Kobayashi E, Ito Y, et al. Localization and health effects
of lanthanum chloride instilled intratracheally into rats.
Toxicol. 1992;
76(2): 141-52.
U.S. Environmental Protection Agency Web site. 2009.
https://www.epa.gov/ground-water-and-drinking-water
Vaziri N. Oxidative stress in uremia: Nature, mechanisms, and potential
consequences. Sem Nephrol. 2004; 24(5): 469-73.
Walton J, Tuniz C, Fink
D, Jacobsen G, Wilcox D. Uptake of trace amounts of aluminum into the brain
from drinking water. Neurotoxicol. 1995; 16(1): 187-90.
Wanamaker BP,
Massey KL. Applied Pharmacology for Veterinary Technicians. Maryland Heights,
MO: Elsevier Health Sciences; 2008.